5.1 Potential Barriers and strategies to overcome these barriers
As highlighted in chapter 1, the integration of digital technologies into rehabilitation presents distinct advantages for health care in East Africa, including the significant potentials of Digital Rehabilitation. Despite the numerous advantages, there are barriers that may not be inherent but can arise in the use of digital technologies. This could lead that Digital Rehabilitation interventions cannot be performed, rehabilitation professionals/clients are less motivated to carry them out, which in turn can weaken adherence to rehabilitation and thus the effect.
The list of barriers does not claim to be exhaustive. If you use Digital Rehabilitation in practice, are planning to use/implement it or are already receiving it as a client, you may notice other barriers. The barriers listed are those most frequently mentioned in the literature in relation to Digital Rehabilitation in Sub-Saharan Africa. Most of the barriers presented in this chapter are based on a scoping review that was conducted as part of this project. You can view the registration of the paper via this link: https://osf.io/xyvmj [1]. The full paper is expected to be published by end of 2024.
Note: The strategies listed below could be possible ways to overcome potential obstacles, but it will require collaboration between governments, healthcare providers, technology developers, and communities to develop sustainable and culturally appropriate solutions that overcome these challenges.
5.1.1. Access to internet
Since the invention of the internet and the development of the first website in 1990, it has developed enormously at a rapid pace. Now we cannot only make information accessible regardless of time and place, but we can also carry out banking transactions and offer rehabilitation services online.
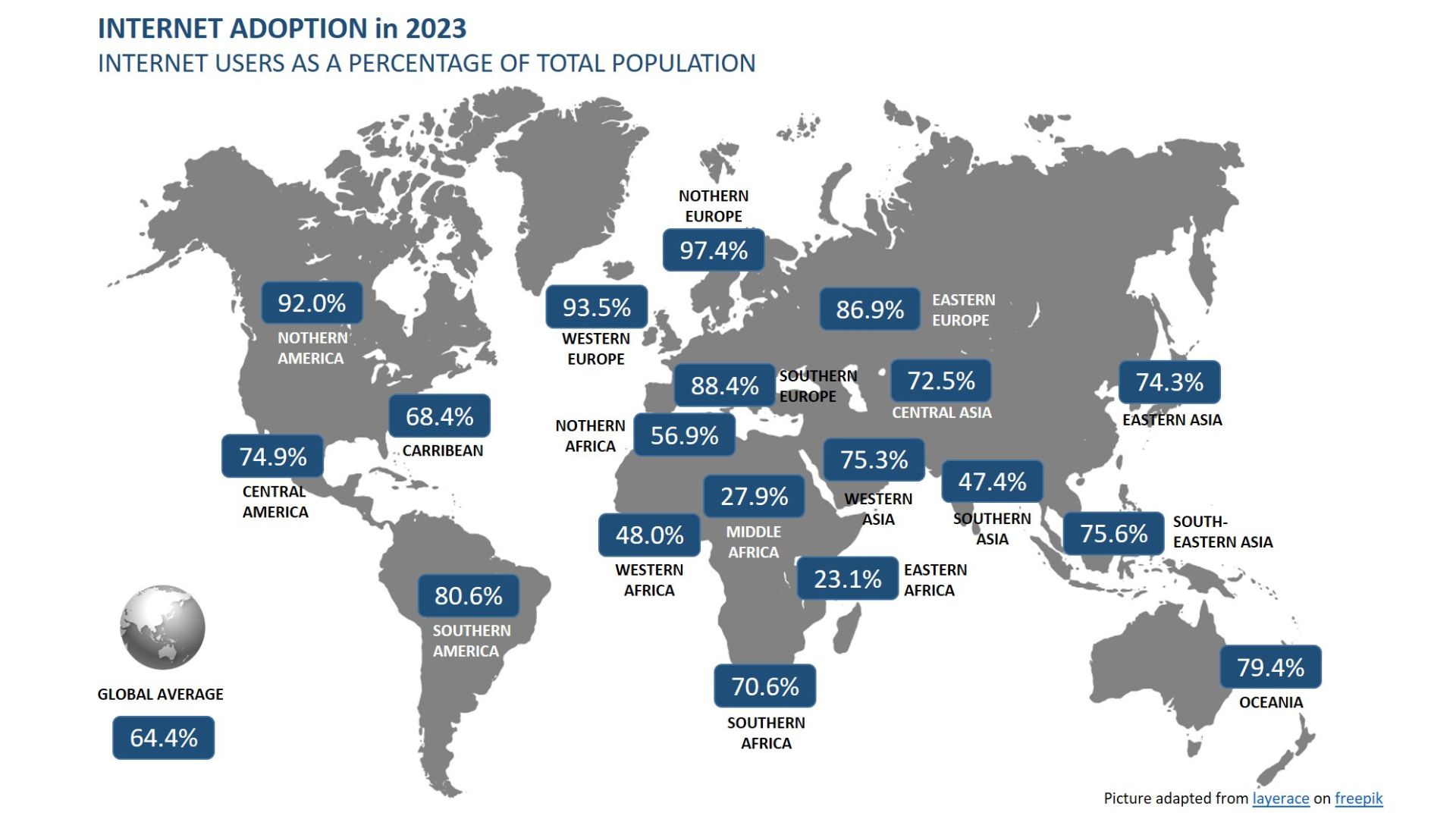
Figure 1. shows the increase of internet users from the invention of the first website in 1991 until 2023 [2].
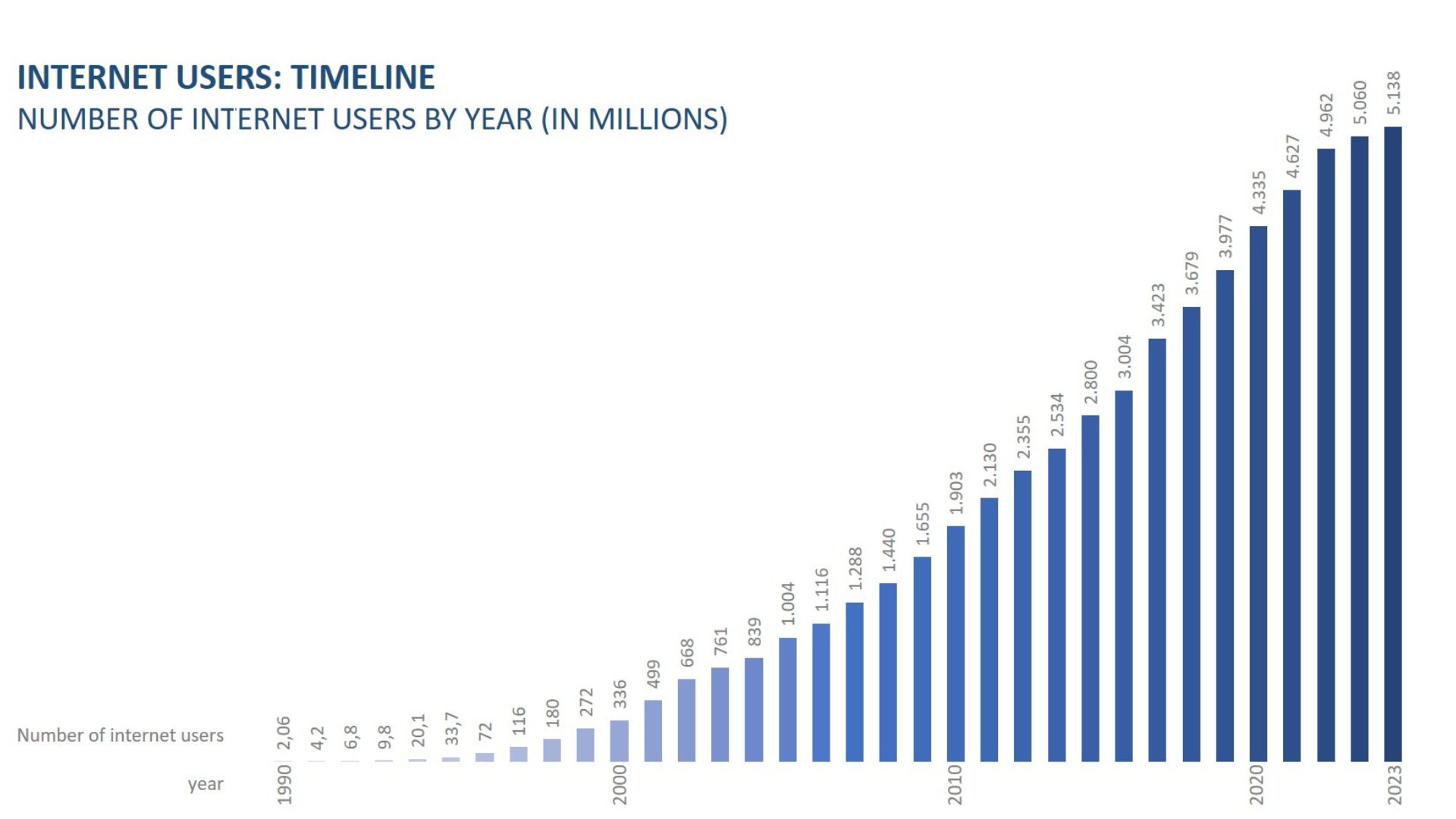
Figure 1. Internet users worldwide from 1990 until 2023.
By 2023, the number of internet users stands at 5.158 million worldwide. However, there is also a discrepancy to the average use worldwide compared to the usage in East Africa. In figure 2 you can see the internet adoption in 2023 worldwide [2].
The number of people who do not use the internet in East Africa is 328.9 million (figure 3) [2]. There are several reasons why many people in East Africa do not use the internet. On the one hand, many people do not have money to access the internet and on the other hand, the coverage of internet is not seamless in some regions in this area.
As an internet connection and coverage is essential for synchronous access to Digital Rehabilitation services, this could limit usage. However, there are some ways to mitigate this challenge now and/or in the future:
Digital services without internet connection
Digital services that are possible without internet connection could be used to enable remote rehabilitation. For example, SMS could be used to provide information about a condition such as depression/diabetes and provide emotional support without the need for the affected person to visit an appropriate facility [3,4]. SMS could also be used to motivate clients to do their exercises at home and remind them of upcoming appointments [5]. Certainly, the functionality and customization potential of SMS services for rehabilitation are constrained. Therefore, an improved approach would involve expanding internet coverage.
Blended interventions
Another strategy could be to offer blended interventions, such as those suggested by Yusuhp et al. [6]. Blended interventions are interventions in which face-to-face sessions are offered in a rehabilitation center/hospital and these are mixed with digital sessions that can be conducted remotely [7]. This means that the client does not have to rely exclusively on digital services if, for example, the client lives in a region where internet coverage is low.
Asynchronous interventions
If the client or rehabilitation professional does not have permanent access to the internet and therefore synchronous digital interventions such as video conferencing are not possible, another solution could be to offer asynchronous rehabilitation content digitally. This means that the rehabilitation provider does not have to be online at the same time as the client. In this way, content can be stored online and accessed by the client at another time remotely. In an example presented by Osborn et al. [8], high-school students with depressive symptoms living in Kenya were able to follow an intervention via a computer program that could be followed by the students in the school they attend. The intervention consisted of reading and writing activities about 3 concepts: growth mindset, gratitude, and value affirmation. The intervention produced greater reduction in depression symptoms.
Investment in infrastructure
Governments, NGOs, and private sector entities can invest in improving internet connectivity and electricity access in underserved areas. This could involve expanding the reach of existing infrastructure or deploying alternative technologies such as solar power or satellite internet.
Supporting digitalization
Political initiatives that also promote digitalization in East African countries, such as the expansion of internet connectivity and/or the development of a digital infrastructure are essential in order to access digital services.
For example, Kenya’s government has developed a digital masterplan [9] that intends to build a robust, secure, affordable, accessible and reliable digital ecosystem, which benefits the public and private sector, and improve quality of life until 2032. This strategy outlines a comprehensive approach to enhance Kenya's digital ecosystem, including the expansion and improvement of digital infrastructure, services, products, and data management. It aims to bolster digital literacy across the population, offer support to enterprises and businesses, and develop legislation and regulations to facilitate digitalization throughout the country. The activities described are not only focused on the health care system but covers all sectors that are affected by digitalization. The plan has not yet been fully implemented and/or evaluated, but it shows that the government is supporting digitization and promoting projects that have the same goal.
Go to chapter 4, to learn more about the specific measures that Kenya, Tanzania and Rwanda take to improve the digital infrastrucutre in these countries.
5.1.2. Access to digital devices
Many Digital Rehabilitation services are offered as an app or as a web-based program. A suitable device is required to access these therapy and training programs. Smartphones are often used for this purpose, as they are portable and can therefore be used regardless of the location. This is a great advantage compared to a computer or laptop. The number of smartphone users is increasing worldwide, as figure 4 shows [10]. According to forecasts, there will already be over 5 billion users by 2028.
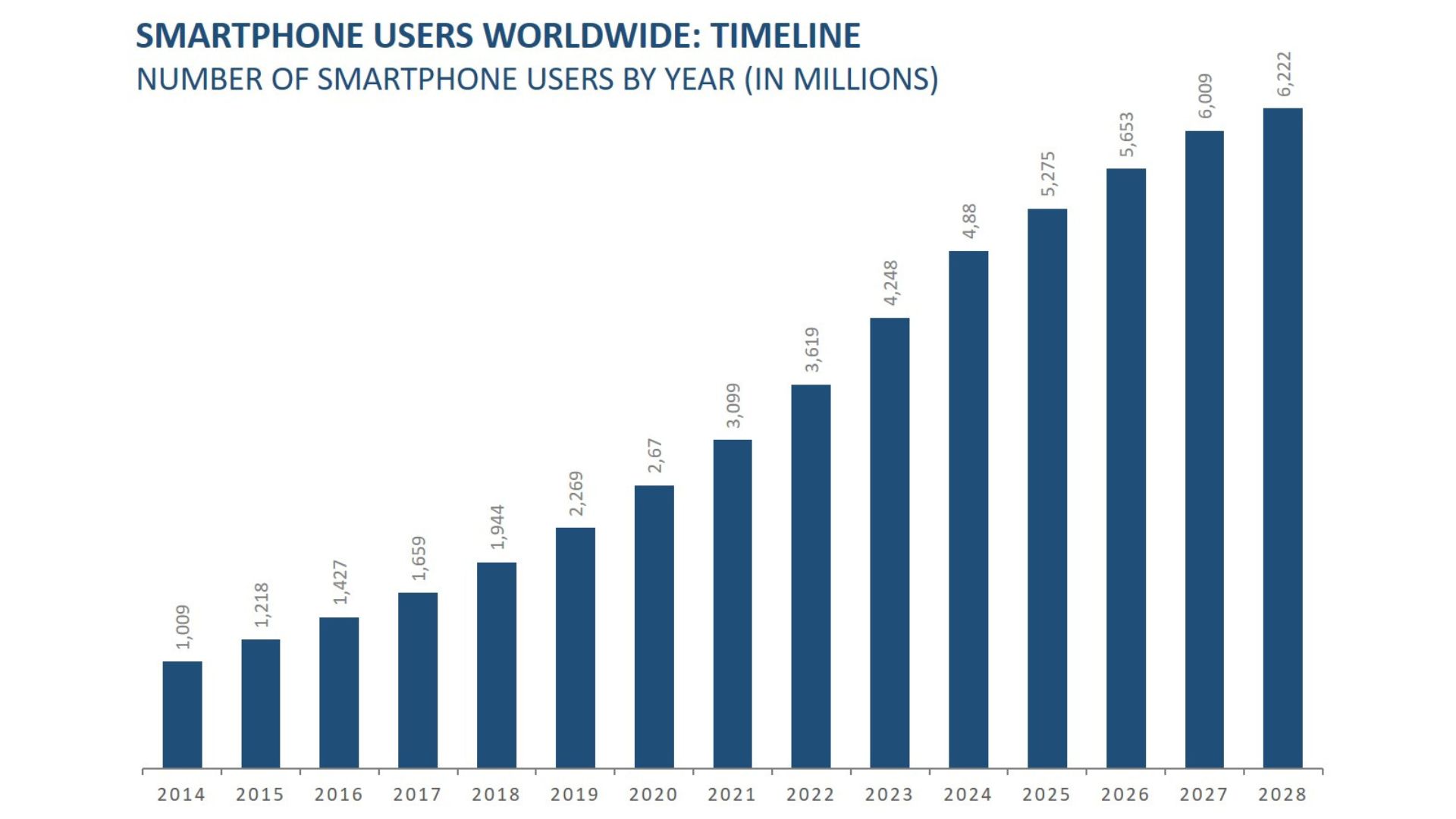
Figure 4. Number of Smartphone Users worldwide from 2013 until 2028 (in millions).
There has also been an increase in smartphone users in the Sub-Saharan Africa region (Figure 5), although the number is said to be only 688.89 million [11]. Even though the number of users has increased enormously in Sub-Saharan Africa, currently not everyone has a smartphone to access Digital Rehabilitation services and/or the money to buy bundles to access internet.
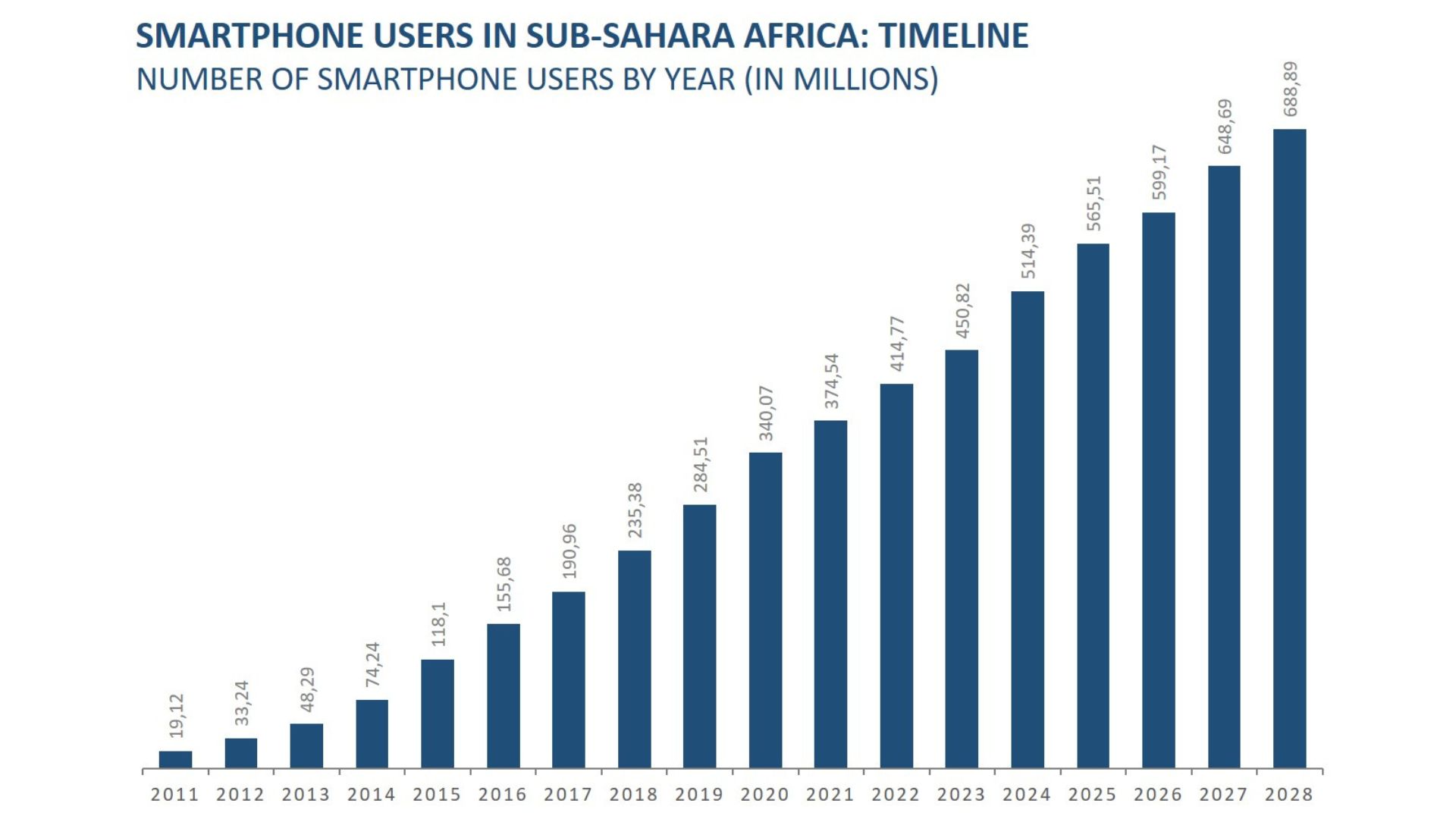
Figure 5. Number of smartphone users in Sub-Sahara Africa from 2011 until 2028 (in millions).
Access via schools
For this potential hurdle, access to digital interventions could be created via laptops/computers that clients can access anyway. For example, it would be possible for students to carry out digital interventions on the computer of the school they attend, as described in the example by Osborn et al. [8]. This would allow clients to benefit from the advantages of digital interventions without owning a mobile device or having a laptop/computer at home.
Access via community
Another approach to equip rehabilitation professionals with the needed equipment (like a tablet) to bring digital interventions to the community. A social worker who is visiting the community on regular base could ask the rehabilitation needs of the community beforehand. Even without permanent internet access, digital interventions could be stored on the social workers tablet and could be offered to the people living in this community. In this way, the interventions could not be individualized but could cover the greatest needs from the community.
5.1.3. Technical issues
Another barrier that can limit the use of Digital Rehabilitation services are technical problems with the internet or smartphone. For example, the smartphone could break down or repairs for the device could take longer, meaning that the client is no longer in possession of the smartphone. In addition, server breakdowns or electricity cut-offs are more common in sub-Saharan Africa, which can also affect usage negatively.
Low-tech options
In areas where server breakdowns and power cuts are more common, it would be beneficial to use low-tech options such as SMS-based platforms or interactive voice response systems that can be accessed with simple mobile phones. Look at the best practice example from Teriö et al. [12] in chapter 2, where the research group used SMS services as an intervention in Uganda to improve physical activity in people with stroke.
5.1.4. Digital (health) literacy
Among the 17 studies included in the scoping review conducted as part of the RADIC project, six specifically assessed the barriers and facilitators for the use of Digital Rehabilitation services in Sub-Saharan Africa. All of these studies identified low digital (health) literacy of both clients and rehabilitation professionals as a significant barrier for the use of Digital Rehabilitation services.
Digital literacy is an individual's ability to find, evaluate, and communicate information using typing or digital media platforms. It is a combination of both technical and cognitive abilities in using information and communication technologies to create, evaluate, and share information. While digital literacy initially focused on digital skills and stand-alone computers, the advent of the internet and social media use has shifted some of
its focus to mobile devices. Digital health literacy refers to the ability to seek, find, understand and appraise health information from electronic resources and apply such knowledge to addressing or solving a health problem [13].
With recent technologies and developments, e.g. in the area of social media and mobile user devices, the requirements for digital skills are also constantly changing. This includes understanding how to use web browsers, features of mobile devices, search engines, email, word processing, wikis, blogs, graphics, videos and presentation software. It also includes the ability to evaluate online resources for the trustworthiness of information. If digital (health) literacy in society is low, it is difficult to implement Digital Rehabilitation services, as the client and/or rehabilitation staff can only use the devices to a limited extent.
Technical support
Providing ongoing technical support to healthcare providers and users is essential for troubleshooting technical issues and ensuring smooth operation of Digital Rehabilitation platforms. This can be done through help desks, online forums, or dedicated support teams. However, this is only a short-term solution, and a more sustainable strategy would lead to better results.
Training
Providing training for healthcare workers and community members on how to use Digital Rehabilitation platforms can help overcome this barrier. This includes training on basic digital literacy as well as specific skills related to using the rehabilitation software such as receiving and sending text messages, searching for useful information on the internet and downloading updates to maintain the security of the device, etc. This would be valuable to the entire population, as digital devices can be used for many purposes. These programs can be delivered through community centers, schools, churches, and other local organizations.
Peer-support
Training community members could also serve as peer educators who can disseminate health information and provide support to their peers. Peer education programs can help foster trust and facilitate the sharing of information within communities.
5.1.5. Acceptance and awareness
There may be a lack of awareness among both healthcare providers and clients about the benefits of Digital Rehabilitation. Resistance to adopting new technologies or skepticism about their efficacy could impede their adoption and usage as described in the papers from Teriö et al. and Pandya et al. [12,14].
To overcome this potential barrier, a comprehensive strategy could include:
Training and Capacity Building
Offering training programs and capacity-building workshops for healthcare providers, community health workers, and rehabilitation professionals to enhance their understanding of Digital Rehabilitation technologies and their integration into practice. Providing hands-on experience and ongoing support to ensure confidence and competence.
Demonstration and Pilot Projects
Implementing pilot projects or demonstration programs in collaboration with local healthcare facilities to showcase the effectiveness and potential impact of Digital Rehabilitation. Collect data and testimonials from participants to demonstrate the benefits and build credibility within the community.
Partnerships with Key Stakeholder
Forge partnerships with government agencies, NGOs, academic institutions, and technology companies to leverage resources, expertise, and networks for promoting Digital Rehabilitation awareness and acceptance. Collaborate on advocacy campaigns and capacity-building initiatives to amplify efforts.
Tailored Messaging and Materials
Developing culturally appropriate educational materials, including brochures, posters, videos, and social media content, to communicate the importance of Digital Rehabilitation in local languages and formats accessible to diverse audiences. Highlight success stories and real-world examples to make the concept relatable and inspiring.
Policy Advocacy and Integration
Advocating for the integration of Digital Rehabilitation into national healthcare policies, strategies, and programs to institutionalize its importance and secure sustainable funding and support. Engaging policymakers and advocacy groups to prioritize digital healthcare initiatives and remove regulatory barriers.
5.1.6. Design of technology
Inadequate design of rehabilitation services, such as poorly designed apps, negatively affects the utilization of technology. This means, for example, if the handling is not intuitive, the user has to spend some time familiarizing themselves with the content, and functions, which will have a negative impact on acceptance by both clients and rehabilitation professionals.
The design of e.g. an app should be tailored to people with physical disabilities. For example, many clients who need rehabilitation have visual impairments, which limits the handling of a smartphone/an app. This problem could be solved by using larger fonts and icons in the applications. There should also be a way for blind people to use an app by embedding an audio guide in the app. As an example: Since the tremor of people with Parkinson's disease are hindered to move their fingers purposefully to the buttons of a smartphone, voice control would help to use a smartphone even if they are limited in their function.
Collaboration
When companies, which are developing digital devices/rehabilitation services, would include clients and rehabilitation professionals in the development of these services they would get vital information about usability aspects. Based on the results, the device/program could then be further adapted and or new functions could be integrated. Involving the target group is essential if we want that people benefit from Digital Rehabilitation.
Universal Design
Guidelines also exist to design digital solutions with respect to the physical conditions, such that as many people as possible, regardless of disability, can use the general functions of the intervention. Read Chapter 7 to learn more about the ”Universal Design” guiding principle, which aims to make digital content accessible to everyone despite physical challenges.
5.1.7. Policies and regulations
Furthermore, the absence of regulations pertaining to Digital Rehabilitation may create hurdles in its implementation. A case in point is the lack of clarity on billing procedures for such services—whether the client's insurance company is responsible for payment or if it falls to the clients themselves. This issue is further compounded in instances where clients lack insurance coverage, presenting an additional challenge.
There is also the possibility that the client may injure themselves during exercises at home when he/she is not under supervision. There are also no regulations who is responsible and bears the consequences.
New regulations
A policy is needed that precisely clarifies such issues and draws up regulations or passes laws accordingly so that there are realistically feasible approaches to implement Digital Rehabilitation nationwide.